
A new analysis of data from Northwestern Medicine found some chronic inflammatory diseases were associated with a 7-fold increase in risk of heart failure.

A new analysis of data from Northwestern Medicine found some chronic inflammatory diseases were associated with a 7-fold increase in risk of heart failure.

The international registry that was created in March to track rheumatology patients who have contracted COVID-19, has released data from the first 110 cases from six continents.

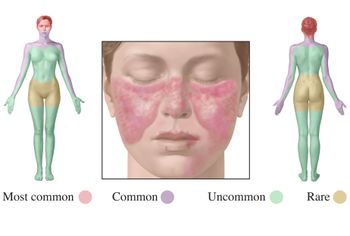
A 16-year-old African American girl reports sudden erythema covering her nose, cheeks, and upper back. Can you diagnose this patient?

The rheumatology community has expressed concerns about the use of hydroxychloroquine sulfate for COVID-19 because the drug is used to treat lupus patients and is already in short supply. The FDA has taken steps to redistribute the drug to hospitals for COVID-19 patients despite the lack of extensive clinical trials testing.

David Karp, MD, PhD, president-elect of ACR discusses what an appropriate hydroxychloroquine trial would look like, alternate treatment options, and how rheumatology experts should approach their patients during this time.
Patients with systemic lupus erythematosus depend on hydroxychloroquine to control disease activity, but demand for this drug, which was already in short supply, has spiked since President Trump championed its use for COVID-19 patients. The American College of Rheumatology has responded by issuing a series of recommendations. Learn more in this article.
In patients with moderate to severe systemic lupus erythematosus (SLE), anifrolumab (AstraZeneca) was superior to placebo for improving overall disease activity, skin disease and oral corticosteroid tapering, say researchers writing in the New England Journal of Medicine.

Anifrolumab, a potential new treatment for systemic lupus erythematosus (SLE), was given a second look in a clinical trial published in the New England Journal of Medicine this month. This time, the results look promising. Learn more about the trial in this slideshow.

In this slideshow, we feature the lupus stories that resonated most with our readers in 2019: Lupus patients are increasingly turning to opioid use to control pain, a study that shows anifrolumab may be the next belimumab for lupus, patients are turning to pill splitting to keep costs down, among others.

Nearly one third of patients with systemic lupus erythematosus use prescription opioids, with around two thirds of those using opioids for more than a year, while emergency department use is associated with increased prescription opioid use, say researchers writing in Morbidity and Mortality Weekly Report in Septmeber.

2019 was a significant year for new developments in the treatment of systemic lupus. These include new treatment options for systemic lupus and updated treatment guidelines for established treatments. In this slideshow, we highlight a few of the achievements made throughout the year.

A large proportion of patients with systemic lupus erythematosus (SLE) have been inappropriately prescribed opioids, researchers reported recently in the Morbidity and Mortality Weekly Report.
Peter Izmirly, MD, discusses the results of a trial he led examining the possible reduction in recurrence of congenital heart block from treatment with hydroxychloroquine at ACR 2019.

Jianmin Fang, PhD, CEO and founder of Remegen Ltd., discusses the results of a phase 2b trial exmaining the use of telitacicept for the treatment of SLE.

ACR Annual Meeting: In patients with moderate to severe systemic lupus erythematosus, anifrolumab (AstraZeneca) was superior to placebo for overall disease activity, skin disease and oral corticosteroid tapering, among other efficacy endpoints, according to a study presented at the annual meeting of the American College of Rheumatology in Atlanta on November 12.
ACR Annual Meeting: At the American College of Rheumatology annual meeting in Atlanta today, Dr. Konstantinos Tselios of the University of Toronto addresses the challenges associated with developing new treatments for systemic lupus.

Patients with lupus were at an increased risk of 30-day all-cause mortality following coronary revascularization when compared to patients with diabetes mellitus and the general population.

Low-dose IL-2 might be effective and tolerated in the treatment of systemic lupus erythematosus (SLE), say researchers writing in Annals of the Rheumatic Disease this month.
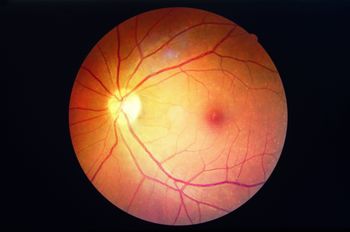
Hydroxychloroquine retinopathy is more common than previously thought, shows a study published in Arthritis and Rheumatology. Higher dosages and long duration of use is associated with a higher risk of vision loss.
While significant advances have been made in the treatment of systemic lupus erythematosus (SLE), the highly variable manifestations of the disease make treatment difficult.

Availability of new dosages for hydroxychloroquine-a first-line therapy for systemic lupus-may be best for patients, shows a survey conducted by the Lupus Foundation of America.

A review in the journal Lupus examines treatments for primary and secondary thromboprophylaxis in patients with anti-phospholipid autoantibodies (aPL) and a history of thrombosis, which can affect more than 50 percent of people with systemic lupus erythematosus.

In a review that examines the use of conventional and orphan autoantibodies as biomarkers for diagnosing systemic lupus erythematosus (SLE), researchers say the science is advancing rapidly with the goal of diagnosing lupus earlier than currently done.
Sjögren’s syndrome secondary to systemic lupus erythematosus (SLE) rises in frequency with age, affects around one-quarter of all people with systemic lupus, and, despite less internal organ involvement than in systemic lupus without Sjögren’s syndrome, is marked by a systemic inflammatory state with high levels of pro-inflammatory cytokines, say researchers writing in The Journal of Rheumatology this month.
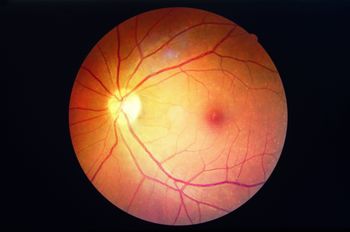
The incidence of retinopathy among systemic lupus erythematosus (SLE) patents treated with hydroxychloroquine increased with longer treatment duration, but could be predicted by monitoring blood levels of the drug, say researchers writing in Arthritis & Rheumatology this month.