
For 2 months, a 29-year-old man had pain and circular, soft swelling (7 x 7 cm in diameter) over the anterior left knee, superficial to the patellar ligament. Pain was minimal and associated with extension and flexion).

For 2 months, a 29-year-old man had pain and circular, soft swelling (7 x 7 cm in diameter) over the anterior left knee, superficial to the patellar ligament. Pain was minimal and associated with extension and flexion).

With the advent of expensive laboratory tests and sophisticated imaging, the diagnosis of rheumatoid arthritis (RA) remains clinical. Because early detection is important for preventing clinical and radiographic progression, revision of the diagnostic criteria was needed and has been implemented.

Gout is a chronic, progressive disease that is managed most effectively when the patient's serum urate level is reduced to lower than 6 mg/dL by early therapeutic intervention.
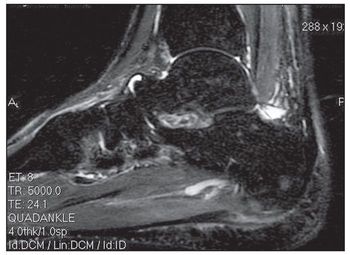
A 31-year-old Asian man presented for evaluation of left foot pain that began on the day before his clinic visit while he was practicing parkour (the physical discipline of training to overcome obstacles within one’s path by using only the human body and objects in the environment). He had no significant medical history. The patient recalled leaping from a platform toward a horizontal bar attached to a wall a few feet away. During the lift-off phase of the jump, he experienced a snapping sensation in his left foot, with subsequent pain in the arch and heel. Immediately after this event, he was unable to ambulate.

Researchers plan to study the effects of hip replacement therapy on the employment and retirement decisions of older adults.

The results of a Brazilian study may help reduce the likelihood of misdiagnosing autoimmune disorder.

Idiopathic inflammatory myopathy is a term applied to a group of relatively rare diseases that present with the gradual onset of weakness of shoulder and pelvic girdle muscles. These diseases include polymyositis and dermatomyositis, as well as myositis associated with neoplastic disease, myositis associated with underlying collagen-vascular disease, and inclusion body myositis.

DISH, a radiographic finding characterized by abnormal calcification and ossification in the axial skeleton and in ligaments and entheses,1 most often affects the thoracic spine. Of note, the findings almost always are more prominent on the right side (the left side may be spared because of aortic pulsations). The enthesopathy, also called“whiskering,” can affect the pelvic brim, ischial tuberosities, greater trochanters, and other features that have ligamentous attachments.2 Diagnosis often is made after an incidental finding in an asymptomatic patient.

Researchers have identified a gene responsible for a rare disease leads to progressive loss of fat and muscle, and joint stiffness. and

A protein identified in a University of Central Florida lab has the power to suppress inflammation.

A 50 year-old physician experienced the abrupt onset of tenderness and swelling in the distal interphalangeal (DIP) joint of his right index finger. His only significant past medical history was Wolf-Parkinson-White syndrome, which was managed successfully with ablation. The same symptoms subsequently occurred in the DIP joints of his left index finger and fifth digits of both hands. No other digits were affected. The symptoms made it difficult for him to type on the computer. He denied trauma to the affected fingers, although he is an athlete and had had a left middle finger avulsion fracture, right middle finger dislocation, and left radial frac-ture. He had no systemic or other joint involvement.

The American College of Rheumatology has put together a list of 13 myths about rheumatoid arthritis.

Back pain patients receive quicker diagnosis and treatment with nurse practitioner first.

Arthritis patients benefit significantly when they receive homeopathy alongside conventional treatment over a period of six months.

A new study suggests joint complaints attributed to the popular breast cancer drugs are not associated with inflammatory arthritis or autoimmune disease.

Revised evidence-based guidelines for non-pharmacologic treatments of osteoarthritis were unveiled at the 2010 Annual Meeting of the ACR.

Basal joint arthritis of the thumb is sometimes misdiagnosed as CTS.

A common pitfall in the diagnosis of osteoarthritis (OA) is misinterpretation of the patient's symptoms and signs.

Research uncovers glucosamine's killing power over pancreatic cells.

Strong, positive marriages can help rheumatoid arthritis patients cope better.

Experts offer recommendations in six key areas to treat rheumatic and musculoskeletal disease.

It is vital that those caring for IBD patients evaluate for vitamin D nutritional deficiency.

Physicians treating patients with fibromyalgia syndrome should rule out coexisting disorders and establish possible inducing factors.

The numerous symptom domains of fibromyalgia syndrome (FMS) include pain, fatigue, sleep disturbance, mood disturbance, and cognitive dysfunction, as well as close association with other “central sensory augmentation” conditions, such as irritable bowel syndrome and various forms of headache.

Varying practitioner beliefs about what makes patients who have fibromyalgia syndrome (FMS) “behave” differently from the general population are complicated by a paucity of studies, heterogeneity of the patient population, and other factors.

Scheduling, event, exhibit hall, CME, and other information for attendees of the 48th Annual Meeting of the Infectious Diseases Society of America.

Despite claims that biologics for treating rheumatoid arthritis are highly effective, Medicaid patients seem to demonstrate low adherence.

Gout is the most common inflammatory arthritis. Arthrocentesis and identification of negatively birefringent monosodium urate crystals from aspirate is the gold standard for diagnosis.

With the rising incidence of obesity and an increasing older population, the burden of osteoarthritis (OA) is expected to grow. Understanding of the disease is limited, and there are indications that many patients are receiving suboptimal care.

The significant changes in the way rheumatoid arthritis has been managed include earlier, more aggressive treatment with combination therapy.